The Pelvic Floor Explained
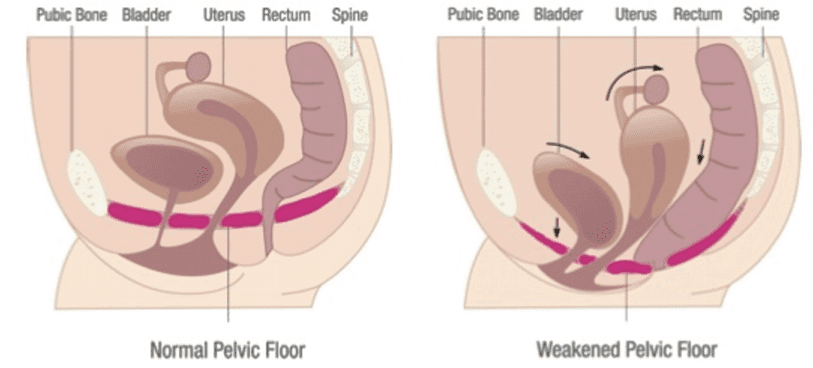
The pelvic floor muscles are a supportive basin of muscle attached to the pelvic bones by connective tissue to support the vagina, uterus, bladder and bowel. The main group of muscles providing this support is called the ‘levator’ muscles. There are also nerves that relax or squeeze these pelvic muscles as needed.1
Between the levator muscles there is an opening that allows the urethra, vagina and back passage to exit the abdomen. This is called the ‘levator hiatus’.
What Happens to the Pelvic Floor During Childbirth?
During a vaginal birth, the baby needs to pass through the ‘levator hiatus’ in the pelvic floor, and the muscles, connective tissues and nerves can be damaged in the process. The levator muscles are stretched by 1.5 to more than 3 times their normal length as the baby passes through, depending on the size of both baby and pelvic floor muscle opening.2,3 In many women, these muscles return to normal but in 10-30% of women the muscles are overstretched or sometimes torn off the bone. This injury is called a ‘levator avulsion’. 4,5
Whether a woman suffers damage to the pelvic floor in labour or not depends on many things. In general, the older a mum is at the time of the first vaginal birth the less the tissues are able to stretch and the greater the chance of injury. Older mums-to-be have a higher rate of caesarean or assisted vaginal delivery, including forceps or vacuum.6 Even if a woman manages to avoid a caesarean, the risk of pelvic floor muscle injury rises by about 10% with every year of delay in having your first child.7 It is also important to note that it’s the first vaginal birth that generally causes the most damage, with the following births having less effect on the pelvic floor supports.8,9 A second vaginal birth without forceps, is unlikely to cause additional damage.8 However, women who have a vaginal birth after a previous caesarean section (VBAC) have higher rates of pelvic floor trauma.
Pelvic Floor Injury After Childbirth
While most perineal injuries usually heal well, the same does not seem to occur with these deeper pelvic floor tears known as levator avulsions. There are many studies tracking the follow-up appointments of women for years after a levator avulsion that show that the muscle has not reattached itself or healed.10
Imaging after childbirth shows that once the muscle is pulled off the bone it shrinks and pulls back towards the back passage. In some women, the avulsion is not complete and scar tissue can bridge a partial tear, but once the muscle is completely off the bone, the defect usually won’t heal.10 In some women, levator avulsion occurs on both sides, and there is even less pelvic floor support remaining. These women can develop pelvic floor problems shortly after birth. This indicates the importance of trying to prevent the tears from happening in the first place.
More Information
The Impact of Levator Avulsion
Until ultrasound could identify these tears, obstetricians and gynaecologists were not aware that they had occurred. In fact, there are tens of thousands of women in the community who have suffered this kind of injury in childbirth without being aware of it. Partly this is because it takes many years of pressure on the pelvis to cause the supports to stretch and cause bladder, bowel and prolapse problems. Also, there are other parts of the pelvic floor that can compensate.
What we can say right now is that pelvic floor muscle trauma (‘avulsion’):
- weakens the muscle by about 1/3 on average.11
- makes the muscle stretchier by about 25%.12
- enlarges the opening of the pelvic floor (the ‘hiatus’).12
- more than doubles the risk of bladder prolapse.13,14
- triples the risk of prolapse of the uterus (the womb).13
- doubles the risk of a prolapse returning after pelvic floor surgery.15
Factors Associated with Increased Chance of Pelvic Floor Injury
The greater the size of the baby (particularly when that weight is over four kilograms) and the longer the baby is pushed against the pelvic floor in the second stage of labour, the greater the chance of pelvic floor injury.16
An occipito-posterior or ‘OP’ presentation (meaning the baby is positioned so its back is along the mothers back) can also increase the chance of pelvic floor damage as the area of the head is larger causing more stretch of the pelvic floor.2
The biggest risk factor for pelvic floor muscle damage, by far, is the use of forceps.17 Some contributing factors in forceps associated pelvic floor trauma include the increased amount of stretch and force enabled by the forceps and the increased speed at which the muscles are stretched. The additional space requirement probably doesn’t matter much.18
Forceps markedly increases the risk of injury to the pelvic floor muscles and anal sphincter.17,19
Symptoms of Pelvic Floor Injury
The most common problems with loss of pelvic floor support and function are leakage of urine (urinary incontinence) and prolapse. The link between stress incontinence (e.g. leaking while coughing, sneezing, and lifting) and levator injury is much less obvious. Urine leakage is very common among women with or without a damaged pelvic floor, and there are many other factors involved.20
Other symptoms of pelvic floor injury include prolapse and faecal incontinence. Prolapse is when the vaginal walls (with the bladder or bowel behind) or uterus comes down to or through the entrance of the vagina and causes a bulge sensation or pressure. Up to half of all women with damage to the muscle around the back passage may have leakage of bowel contents in the medium term.21
It is important to note that while these symptoms are common with levator avulsion, they are not always coexistent. There are other factors like weak pelvic floor muscles or chronic straining and lifestyle factors that can also lead to prolapse and faecal incontinence.
Pelvic Floor Muscle Damage and Sexuality
Finally, how much does over-stretching or tearing of this muscle affect sexual function? Some women and their partners notice a big difference after the birth of their first child. Others don’t notice anything. In some women, there may be a loss of sensation due to vaginal laxity. Others may experience pain related to the vaginal injury and/or repair. The good news is the levator avulsion does not affect the clitoris. So women’s ability to feel pleasure and orgasm from clitoral stimulation remains unaffected.
On average, women feel that there is more laxity and less muscle strength in the vagina after childbirth.22 Sometimes this leads women to seek help from gynaecologists, who may or may not be aware there is levator injury underlying their symptoms. Surgeons may suggest a range of vaginal surgeries, however, it is almost always worth pursuing non-surgical options with the guidance of your treating clinician, as the first step.22 Pelvic floor physiotherapists have expertise in assessing sexual dysfunction and providing evidence-based management to accommodate the changes and help improve sexual function.